AnatomyPage
1
1
Slide 1
Anatomy
A thorough understanding of the anatomy of the eye, orbit, visual pathways, upper cranial nerves, and central pathways for the control of eye movements is a prerequisite for proper interpretation of diseases having ocular manifestations. Furthermore, such anatomic knowledge is essential to the proper planning and safe execution of ocular and orbital surgery.
Slide 2
The Ocular Adnexa
Eyebrows
Eyelids
Lacrimal Apparatus
Slide 3
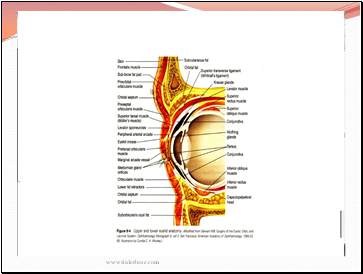
Eyelids
Slide 4
From superficial to deep, they are the skin layer, a layer of striated muscle (orbicularis oculi), areolar tissue, fibrous tissue (tarsal plates), and a layer of mucous membrane (palpebral conjunctiva)
Slide 5
Slide 6
Slide 7
Lid Margins
Anterior Margin
Eyelashes
Glands of Zeis
Glands of Moll
Posterior Margin
small orifices of modified sebaceous glands (meibomian, or tarsal, glands).
Slide 8
Orbital Septum
the fascia behind that portion of the orbicularis muscle that lies between the orbital rim and the tarsus and serves as a barrier between the lid and the orbit.
Slide 9
Lid Retractors
The lid retractors are responsible for opening the eyelids.
In the upper lid: levator palpebrae superioris & Muller's (superior tarsal) muscle
In the lower lid:the main retractor is the inferior rectus
The smooth muscle components of the lid retractors are innervated by sympathetic nerves.
The levator and inferior rectus muscles are supplied by the third cranial (oculomotor) nerve. Ptosis is thus a feature of both Horner's syndrome and third nerve palsy
Slide 10
Sensory Nerve Supply
first and second divisions of the trigeminal nerve (V).
Slide 11
Blood Supply & Lymphatics
the lacrimal and ophthalmic arteries by their lateral and medial palpebral branches.
Venous drainage from the lids empties into the ophthalmic vein and the veins that drain the forehead and temple
Contents
- Anatomy
- The Ocular Adnexa
- Eyelids
- Lid Margins
- Lid Retractors
- Sensory Nerve Supply
- Blood Supply & Lymphatics
- The Lacrimal Apparatus
- The Orbit
- Orbital Walls
- Orbital Apex
- Blood Supply
- The Extraocular Muscles
- Nerve Supply
- The Conjunctiva
- Blood Supply& Nerve Supply
- Tenon's Capsule (Fascia Bulbi)
- The Sclera & Episclera
- The Cornea
- The Uveal Tract
- Iris
- The Ciliary Body
- The Choroid
- The Lens
- The Retina
- The Vitreous
- The External Anatomic Landmarks
- The Optic Nerve
- The Optic Chiasm
Last added presentations
- Newton's laws of motion
- Sound
- Direct heat utilization of geothermal energy
- Practical Applications of Solar Energy
- Madame Marie Curie
- Solar Energy
- Soil and Plant Nutrition